Abstract
BACKGROUND Diffuse Large B Cell Lymphoma (DLBCL) is the most common subtype of Non-Hodgkin Lymphoma worldwide. (Blood PMID: 9166827) Treatment survival remains heterogenous due to biologic differences and racial disparities. Multiple epidemiological studies have evaluated racial differences, with heterogenous results (Leuk Lymphoma PMID: 7940576) including the AYA population (Cancer Epidemiol PMID 34597882) with some studies indicating no outcome disparities (Cancer Epidemiol PMID: 28463808) and other showing worse survival in low socioeconomic status including the Hispanics. (HI) (Blood PMID: 24705494) The need of larger studies to characterize survival differences establishes the basis of our nationwide population-based study of DLBCL in HI vs Non-Hispanics (NH).
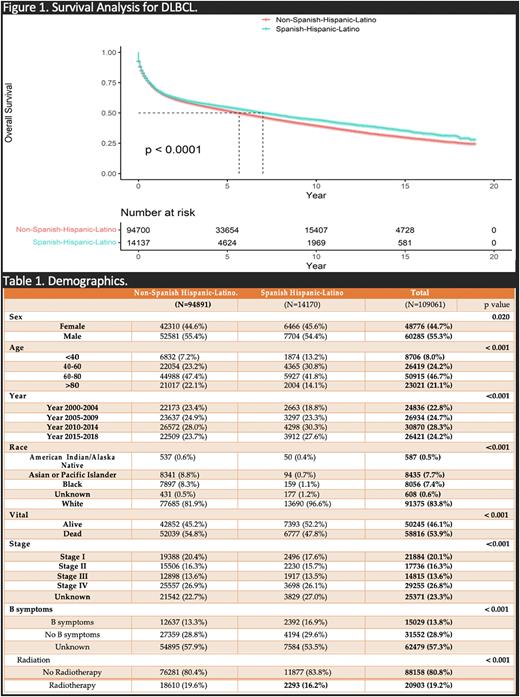
METHODS Data were analyzed on DLBCL patients in the United States (US) reported to the Surveillance, Epidemiology, and End Results (SEER) 18 database between 2000 and 2018. SEER 18 contains the most comprehensive population-based cancer information in the US, covering approximately 27% of the total US population, and up to 36% of HI alone. Racial groups analyzed included NH whites, HI whites, blacks, and Asians/PIs (Pacific Islanders). Patient characteristics, age-adjusted incidence rate, and survival rate were compared across ethnic groups, HI vs NH. Stratification by age, gender, and stage at diagnosis was considered. Kaplan-Meier and Cox regression analyses were used to compare overall survival (OS) between HI and NH. Multivariate analysis and propensity score matching were performed with adjustment for age, stage and B-symptoms.
RESULTS Of 109061 patients with DLBCL, 13% were HI, and 87% NH. 54% of HI were male, compared to 55.4% of NH. The majority of HI (41.8%) were diagnosed in the age bracket of 60-80 years as well as the majority of NH (47.4%) who were diagnosed in the same age bracket of 60-80 (p<0.001). HI were younger at diagnosis, with median age 62 y.o vs 69 y.o in the NH counterpart (p<0.001). Regarding race, most of HI and NH were whites (97% vs 82%), followed by blacks (1% vs 8%). When examining stage, the most common stage for both HI (26%) an NH (27%) was stage IV (p<0.001). In terms of radiation, 16% of HI received it, compared to 20% of NH (p<0.01). On survival analysis, the survival probability at 2, 5 and 10 years of HI vs NH were (62% vs 61%), (54% vs 51%), and ( 44% vs 39%), respectively. The median survival time was 7 years for HI, vs 5.7 years for NH; and there was an OS difference favoring HI with (p<0.0001). On multivariate analysis, when adjusted for age, those patients who were older than 80 y.o and between 60 to 80 y.o, had worse OS compared to those younger than 60 y.o, with HR 5 (95% CI: 4.9 - 5.2 ) and 2.2 (95% CI: 2.1-2.3) respectively. Regarding stage, those who were at stage III and IV, had worse OS than those at early stage (I/II) with HR 1.4 (95% CI: 1.36 - 1.5) and HR 2 (95% CI: 1.9 - 2.1), respectively.
CONCLUSION In this data analysis from the SEER 18 database, HI with DLBCL have dissimilar outcomes when compared to NH. There were statistically significant differences between HI and NH patients in median age at diagnosis, stage, presence of B symptoms and radiation therapy. There were statistically significant differences in median OS, and survival at 2, 5, and 10 years favoring the HI cohort. Unique and heterogeneous characteristics from HI may explain why there is an increase in OS after a DLBCL diagnosis. Further studies aiming at biologically characterize HI with DLBCL are needed to better understand improved outcomes on this cohort.
Disclosures
Diaz Duque:Astra Zeneca: Consultancy; ADCT: Consultancy; Morphosys: Consultancy; Incyte: Consultancy; Epizyme: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal